The Association of Minimally Invasive Gynecologic Surgeons
…dedicated to safe, state-of-the-art surgery and health life-styles for women of all ages
R. Wayne Whitted MD, MPH
Paul A. Pietro MD
8740 N Kendall Dr. Suite 101
Miami, Florida 33176
Phone: 305-596-3744
www.floridaamigos.com
Minimally Invasive Surgical Procedures for Women
Modern advances in surgical technique have rapidly changed women’s health
care. Traditionally, the sole solution to treating specific internal medical problems
was to perform invasive surgery, which involved a large abdominal incision and a
painful and lengthy recovery. Now, accomplishing the same goal with less
invasive procedures has become an alternative for countless women, and the
result is a shorter hospital stay and a quicker and less painful recovery. These
advanced methods result in minimal operative trauma to the surgical area’s skin
and muscles and little or no post-operative scarring. The workhorse of these
minimally invasive procedures is the laparoscope or Hysteroscope, which are used
for both diagnostic screening and operative procedures.
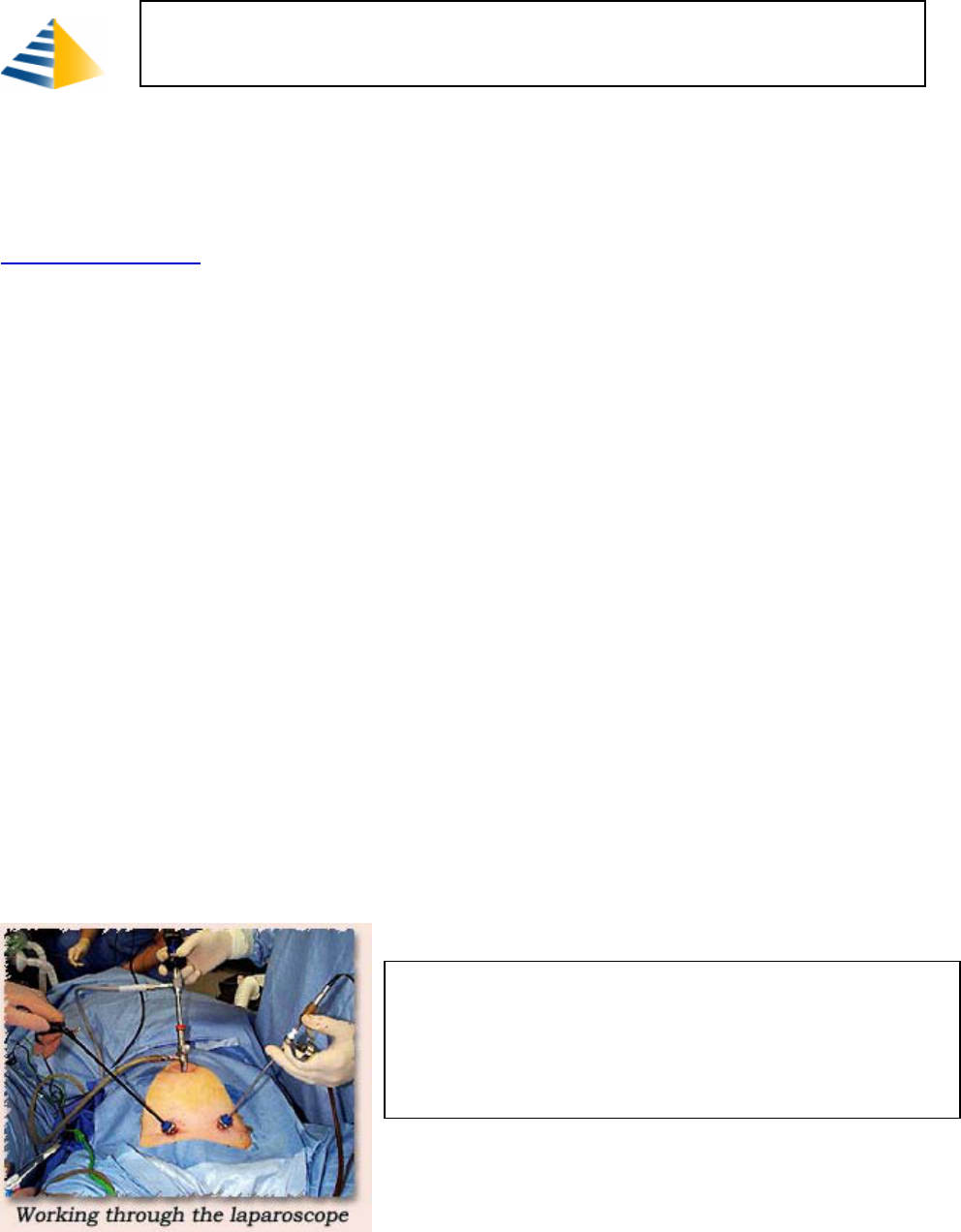
Laparoscopic surgery involves tiny ¼ inch abdominal wall incisions, through
which a harmless gas, e.g. carbon dioxide, is introduced to expand the abdomen,
and create a larger and more visible work area for the surgeon. A tiny lit
telescopic camera (laparoscope) is then inserted through another abdominal
incision. The camera is attached to a television monitor, which allows a physician
to visualize the pelvic organs. Then long narrow surgical instruments are inserted
through another incision, and, with the help of a video monitor, the surgeon is
able to manipulate the instruments and perform surgery.
Gynecologists trained and certified in advanced laparoscopy routinely use
this procedure to treat women’s health conditions, such as infertility,
pelvic pain, endometriosis, pelvic adhesions, fibroids, incontinence and
ovarian cysts.
Since the laparoscope permits pelvic visualization for
simple or advanced procedures, major and minor surgery can be
performed laparoscopically. Laparoscopy is also important in the
diagnosis and treatment of endometrial and ovarian cancers, as well as
other malignancies.
Some of the gyn procedures performed laparoscopically (through tiny abdominal
incisions) or hysteroscopically (through the vagina) are:
• Transvaginal hysterectomy: removal of the uterus and cervix, and possibly
the fallopian tubes and ovaries
• Supracervical hysterectomy: removal of detached uterus through a
laparoscopic incision, leaving a portion of the cervix
• Myomectomy: removal of fibroids from the uterine wall through a
laparoscopic incision
• Tubal ligation: blocking, for sterilization, both fallopian tubes by tying,
sealing or attaching a ring or a clip.
• Reverse tubal ligation
• Ovarian cystectomy: removal of ovarian cyst(s) through a laparoscopic
incision. Laparoscopy is considered an excellent procedure for diagnosing
and treating non-cancerous ovarian cysts
• Infertility: removal of infertility causing endometriosis or pelvic adhesions
through a laparoscopic incision
• Incontinence: anchor bladder neck and urethra to treat stress incontinence
laparoscopically
• Pelvic Reconstruction: repair of uterine prolapse, bladder prolapse, vaginal
prolapse with the laparoscope
Laparoscopy is used to cut or cauterize scarring or growths caused by
endometriosis. Laparoscopic surgery may be required when there is a large
amount of endometrial tissue outside of the uterus or when this tissue covers the
ovaries and interferes with egg production.
Most women who have a laparoscopic procedure are able to go home the same
day. The main benefits of laparoscopic surgery are:
• Less invasive
• Less risk with properly trained surgeon
• Less blood loss
• Less adhesions (scarring)
• Less pain
• Quicker recovery
• Small incisions
• Same day or overnight surgery stay
• Quicker return to work
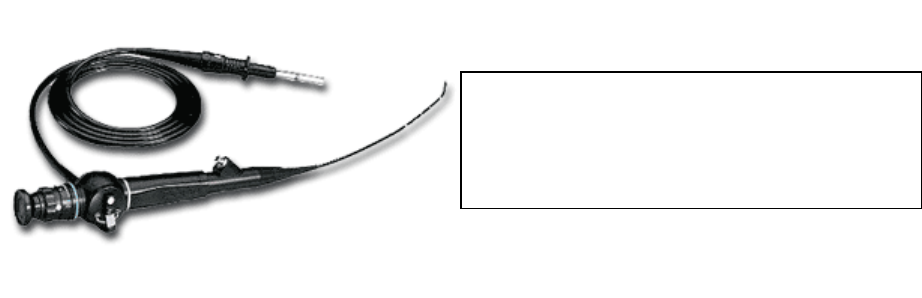
Diagnostic hysteroscopy is the use of a telescopic video camera to visually
inspect, diagnose and treat problems affecting the lining of the uterus
(endometrium) such as polyps, fibroids and anomalies. A physician, guided by
the hysteroscope, can remove polyps and fibroids, correct uterine abnormalities
and remove the lining of the uterus. A hysteroscopy requires general or regional
anesthesia and can be performed as an outpatient procedure. Recovery is related
to the extent of surgery.
The majority of general women’s surgical procedures performed in a modern
hospital setting can be conducted laparoscopically. This reality provides women
with more choices to manage specific gynecologic problems. In other words, the
more a woman knows about these options, the more likely she will make the best
surgical choice in cooperation with her physician.
All About Hysteroscopy
What Is a Hysteroscopy?
Hysteroscopy is a non-invasive (no incisions) diagnostic or operative
procedure, which utilizes a hysteroscope - a thin-lit telescopic device inserted
through the vagina and cervix - to view inside the uterine cavity. It is used to
evaluate patients with infertility, recurrent miscarriages or abnormal bleeding
and to diagnose abnormal uterine conditions, such as fibroids, scarring, polyps
and cancerous or precancerous growths. Hysteroscopy can be used to confirm
the results of other tests, such as a hysterosalpingography (x-ray of uterus and
fallopian tubes).
Diagnostic Hysteroscopy
The first step in a diagnostic hysteroscopy involves slightly widening the
cervical canal with a series of dilators. Once the cervix is dilated, a
hysteroscope is inserted through the cervix and into the lower end of the
uterus. Carbon dioxide gas or special clear solutions are then injected into the
uterus, through the hysteroscope, to expand the uterine cavity, clear blood and
mucous and enable the physician to directly view the internal structure of the
uterus.
Diagnostic hysteroscopy is usually conducted on an
outpatient basis without anesthesia and is usually
performed soon after menstruation, since the uterine
cavity is more easily evaluated and there is no risk of
interrupting pregnancy.
Operative Hysteroscopy
Operative hysteroscopy can be used to treat many of the abnormalities found
during diagnostic hysteroscopy. Treatment may be performed at the same
time as a diagnostic hysteroscopy or at another time. Operative hysteroscopy
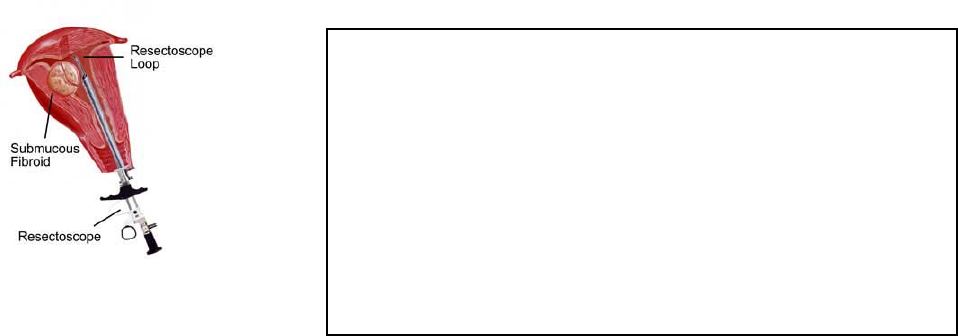
is similar to diagnostic hysteroscopy, except that the hysteroscope is used to
allow operating instruments such as scissors, biopsy forceps and electrosurgical
or laser tools into the uterine cavity via a channel in the hysteroscope. Fibroids,
scar tissue and polyps are then removed from inside the uterus.
Some of the gyn procedures performed hysteroscopically are:
• Hysteroscopic Resection of Sub mucous Fibroids Hysteroscopic
removal of fibroid located in the uterine cavity is extremely efficient
technique with excellent results in experienced hands.
• Hysteroscopic Lysis of Endometrial Scar Tissue
• Hysteroscopic Tubal Obliteration Ligation
• Hysteroscopic Tubo-Cornual Canulation
• Hysteroscopic Septum Resection
Endometrial ablation: electro-, thermal or microwave scarring of uterine lining
through a hysteroscope inserted into the uterus. This procedure can be used
to treat excessive uterine bleeding as an alternative to hysterectomy
Patients normally recover within 24 hours following most hysteroscopic
procedures, which is significantly less than the recuperation period for major
abdominal surgery. Hysteroscopy also decreases patient post-operative
discomfort. . Antibiotics and/or hormonal medication may be prescribed after
surgery to prevent infection and stimulate healing.
Conclusion
Diagnosing and correcting gynecologic disorders once required major surgery
and many days of hospitalization. Minimally Invasive Gynecologic Surgery now
allows physicians to diagnose and correct many of these problems on an
outpatient basis. Before undergoing any surgery, patients should discuss any
concerns about their condition and the procedure to improve their condition
with their health care provider.
Very Truly Yours,
Drs. Whitted and Pietro
The Association of Minimally Invasive Gynecologic Surgeons