The Association of Minimally Invasive Gynecologic Surgeons
…dedicated to safe, state-of-the-art surgery and health life-styles for women of all ages
R. Wayne Whitted MD, MPH
Paul A. Pietro MD
Marina Santana MMS, PA
8740 N Kendall Dr. Suite 101
Miami, Florida 33176
Phone: 305-596-3744
PMS: Sorting Fact from Fiction
There is probably not a woman in the country who does not know what the initials PMS stand for; and few are the women who have
been completely spared the physical and behavioral changes that characterize Premenstrual Syndrome (PMS). Estimates of the
number of women affected by PMS vary widely. The American College of Obstetricians and Gynecologists suggests that 20 to 40
percent of women experience some premenstrual difficulties, while an estimated 5 percent suffer from the depressive illness called
Premenstrual Dysphoric Disorder (PMDD). Some medical experts maintain that up to 90 percent of American women experience one
or more symptoms of PMS. Whatever the actual figures, women and their doctors agree that the problem is real.
PMS symptoms can begin anytime after ovulation, which occurs approximately 2 weeks before the start of your period. During the last
three to 14 days of your cycle, you may notice a variety of changes in your body or disposition that can cause some degree of
distress. These include:
• swelling and tenderness in the breasts;
• a "bloated" feeling or temporary weight gain of a few pounds;
• skin blemishes or acne;
• swelling of hands and feet;
• headaches;
• nausea or constipation, followed by diarrhea at the onset of menstruation;
• increased thirst or appetite;
• a craving for certain foods—especially sweets and items high in salt;
• increased irritability or mood swings;
• insomnia or fatigue;
• forgetfulness or confusion;
• feelings of anxiety or loss of control;
• sadness or uncontrolled crying.
Overall, more than 150 physical and behavioral symptoms have been associated with PMS. This complicates diagnosis and makes it
difficult to classify the condition as a specific disease. And the mild premenstrual changes that many women experience have added to
the confusion over PMS. Multiple severe symptoms that persist over a period of days, month after month, are more likely to be
recognized as PMS than a single symptom or infrequent complaints. In addition, because the variety of symptoms and their causes are
not well understood, doctors have no reliable method to determine who is susceptible to PMS, and why.
Unrelated medical problems can also mimic PMS and mislead you and your doctor. These include:
• fibrocystic breast changes, in which noncancerous lumps in the breast become swollen and painful;
• endometriosis, in which tissue from the lining of the uterus can cause pain elsewhere in the lower abdomen;
• unrecognized pelvic infections such as chlamydia;
• dysmenorrhea, or painful menstrual cramps, that can also prompt nausea and diarrhea;
• diabetes, which can cause excessive thirst or hunger;
• endocrine disorders such as an overactive thyroid;
• emotional or psychological disorders, which can be confused with the mood changes of PMS;
• allergies.
In recent years, PMS has generated a great deal of controversy in the media. While some physicians and researchers have portrayed
nearly all women as suffering from PMS, generally the medical community acknowledges a significant difference between the more
serious "syndrome" and the PMS "symptoms" experienced by many women.
Unfortunately, the politics of the debate have deflected attention from the very real difficulties caused by PMS. While some of the
outbursts attributed to PMS have been casually dismissed as "raging hormones," family, social, and work relationships may, indeed,
suffer when a woman experiences the physical discomfort and emotional peaks and valleys of PMS. Truly violent tendencies, however,
are usually caused by psychological or medical problems completely unrelated to PMS.
In fact, the most convincing evidence of PMS is its cyclical nature. All symptoms—both physical and behavioral—should disappear
rapidly once menstruation begins. If physical changes continue for more than a few weeks or fail to subside once your period begins,
it's important to contact your doctor to rule out other possible medical causes. Likewise, if you feel depressed premenstrually and your
mood doesn't lift when your period starts, you should bring this to your doctor's attention.
No Explanation Yet
The term premenstrual syndrome was coined in 1931, when researchers first suggested that the condition was due to a hormonal
imbalance related to the menstrual cycle. More recent studies have documented that PMS does, in fact, occur only during the
childbearing years between puberty and menopause and subsides during pregnancy. PMS can also affect women who have had their
uterus removed, leading researchers to conclude that the uterus is not part of the problem.
Despite these clues and the recognition of PMS as a legitimate medical concern, researchers have been unable to find a cause. Even
today, no one knows for certain what triggers PMS, though a number of theories have been advanced.
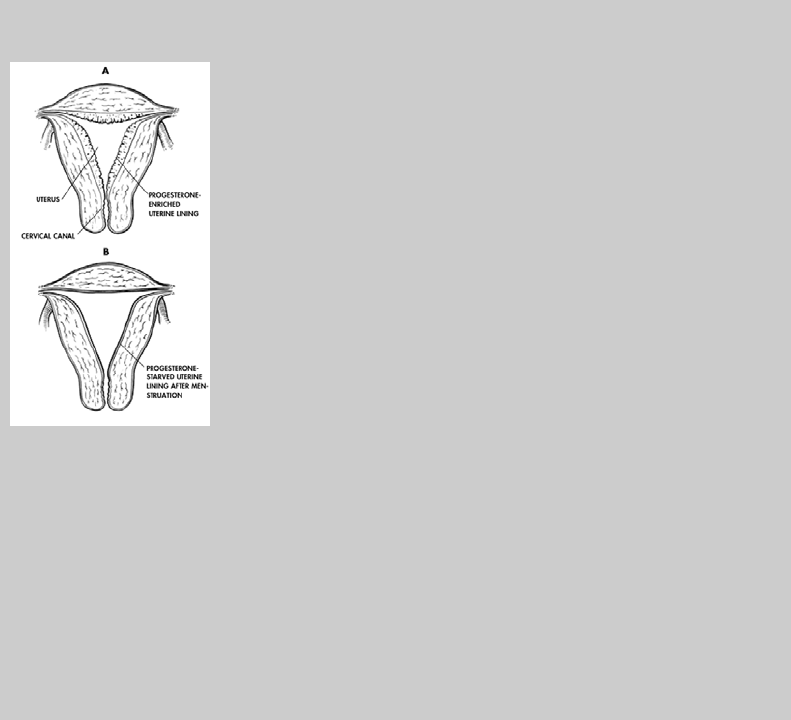
Much of the research has focused on the hormones estrogen and progesterone, which are produced by the ovaries and are known to
interact with certain brain chemicals. At about day 5 of the menstrual cycle, estrogen signals the lining of the uterus to grow and
thicken, in preparation for receipt of a fertilized egg. Once an egg is released from one of the ovaries at mid-cycle, about day 14 of a
28-day cycle, progesterone production begins, causing the release of nutrients and the swelling of blood vessels to prepare for
pregnancy. If the egg is not fertilized, the uterine lining and the egg are shed in menstruation.
The Progesterone Connection
PMS coincides with the final enrichment of the uterine lining in preparation for arrival of a fertilized
egg (see "A" at left). Not coincidentally, this phase of the lining's growth depends on increased levels
of the hormone progesterone, which begins to appear as soon as an ovary releases its egg.
In addition to its effect on the uterus, the extra progesterone is thought to have a damping effect on
certain chemicals in the brain, possibly accounting for the agitation and mood swings that often
accompany PMS. But the connection—if there is one—is still far from clear. Many doctors find that
additional progesterone, taken as a daily shot or suppository, helps to reduce symptoms of PMS.
Whatever the truth of the matter, this much is certain: If conception fails to occur, progesterone
levels decline precipitously, and the hormone-starved uterine lining sloughs off in the monthly
menstrual flow. During the following 2 weeks, when progesterone levels are low and the lining is
relatively lean (see "B" at left), PMS symptoms generally abate.

Thus, estrogen, which interacts with important brain chemicals affecting your mood and energy, dominates the first half of the
menstrual cycle, while progesterone, which tends to suppress the actions of these brain chemicals, is more prevalent during the
second half. Researchers found that temporarily reducing levels of both hormones in a group of PMS sufferers relieved their
symptoms—and that reintroducing the hormones prompted a return of the symptoms.
Still, even though the hormones appear to be a contributing factor, they are not believed to be the actual cause of PMS. Levels of the
hormones seem to be normal in women who suffer the problem. And to confound the issue further, one major study found that
women with PMS continued to show symptoms even after their menstrual cycles were artificially "reset" with medication. Researchers
are studying the possibility that some unknown outside factor disrupts the normal interaction of estrogen and progesterone with
chemicals made in the brain to cause some PMS symptoms.
One theory links fluctuations in the levels of serotonin with PMS. Serotonin (a byproduct of L-tryptophan, an essential amino acid
found in many foods) plays several important roles in the body: it helps regulate sleep and menstrual cycles as well as the appetite.
Some researchers speculate that low levels of serotonin may underlie PMS, throwing off the delicate timing of ovulation and prompting
the restlessness and food cravings so often experienced by women with PMS.
Other theories proposed by researchers include: a deficiency of endorphins, the chemicals in the brain that create a "natural high";
defects in the metabolism of glucose or vitamin BB
6
; low concentrations of zinc in the blood; fluctuations in prostaglandins, a family of
hormone-like compounds found in most body tissue; low magnesium levels; an imbalance in the body's level of acidity; and chronic
candidiasis, a vaginal yeast infection.
As of yet, little conclusive evidence exists to support any of these theories, making a definitive cure difficult, if not impossible. But
research has shown that PMS responds well to a variety of treatments and that most women can minimize its effects by understanding
and carefully managing their symptoms.
Deciding Whether You Have It
The first step toward effective treatment is to confirm that your symptoms actually are caused by PMS. This is usually done by process
of elimination, as there are no reliable tests to diagnose the condition.
Your doctor may first recommend some simple laboratory tests, such as blood tests or urinalysis, to rule out other conditions with
similar symptoms, particularly diabetes or thyroid problems. If you regularly experience pelvic pain, your doctor may check for the
presence of sexually transmitted diseases such as gonorrhea or chlamydia. You should also receive a thorough physical examination,
including breast and pelvic exams, to rule out other undiagnosed medical conditions.
Collecting the Evidence
Mark your calendar on the day your period starts as Day 1. Number each subsequent day and use a
letter code such as "A" for anger, "B" for breast tenderness, "C" for cravings, or "F" for fatigue to
record any symptoms on the days they occur. You can use capital letters if the symptoms are severe
and small letters if they're moderate, or use letters in combination with a rating scale of 1 to 10 to
indicate mild to severe. Additional details to record include your daily weight and, to pinpoint when
ovulation occurs, your basal temperature, taken after you wake up but before you get out of bed.
Your local pharmacy should stock a basal thermometer.
Alternatively, design a simple chart that lists all of your symptoms down one side of a page and the
days of your menstrual period across the top. Fill in the boxes that correspond with a given
symptom and the day of your cycle in which it occurs. On days that you experience only mild
symptoms, color in half the box.
The next step in establishing a diagnosis is to record your symptoms over a period of time to verify their appearance, severity, and
duration. In fact, the only way PMS can be accurately diagnosed is by keeping a careful record of when each symptom appears each
month. Simple record-keeping can be done with an ordinary calendar. See the nearby box on "Collecting the Evidence" for two
methods.
It also helps to keep a diary that describes not only your symptoms but also their effect on your daily activities. Feelings of social
withdrawal, outbursts at family members or co-workers, or difficulties in coping can be more thoroughly described in such a journal.
It's important to maintain your records for at least three menstrual cycles. Record your entries every day, while the symptoms and
their effects are fresh in your mind. You and your doctor can then review the charts and journal to help determine whether you have
PMS and the extent to which it affects your life.

Simple Steps You Can Take Yourself
After you've been able to document the cyclical nature of your symptoms and their severity, you and your doctor can develop a
treatment plan. Your doctor may first recommend simple lifestyle changes, since PMS often responds remarkably well to modifications
in eating habits, stress management, and increased amounts of sleep or exercise.
Caffeine is a major culprit of PMS symptoms. Found in a variety of substances—coffee, tea, soft drinks, chocolate and some over-the-
counter medications—caffeine is a stimulant that is often consumed precisely for the "lift" it provides. Nevertheless, caffeine can
exaggerate PMS-related problems such as anxiety, insomnia, nervousness, and irritability, and it can interfere with carbohydrate
metabolism by depleting your body of B vitamins. Reducing your caffeine intake is a smart move to counteract PMS symptoms and
can provide almost instant relief. In fact, some doctors routinely advise eliminating caffeine from the diet before every menstrual
period as a first step in coping with PMS.
Many women with PMS gain several pounds during the two weeks preceding their period, much of this in fluid weight. Avoiding salty
foods can dramatically reduce bloating and water buildup, resulting in less breast and abdominal tenderness and less swelling in the
hands and feet. Since brain cells also have a tendency to retain fluid, you may find that a salt-free diet eliminates or curbs headaches
and allows you to concentrate better.
PMS or PMDD?
PMS has been linked to serious psychological problems in a small group of women. In Great Britain,
women have been acquitted of various crimes on the grounds that the PMS from which they were
suffering at the time of their action caused a temporary psychiatric disturbance. Though PMS is not
recognized as a valid legal defense in the United States, the American Psychiatric Association (APA)
recognized the possible psychiatric implications of PMS when it classified the related Premenstrual
Dysphoric Disorder (PMDD) as a "depressive disorder not otherwise specified," and included it in the
appendix of the APA's Diagnostic and Statistical Manual of Mental Disorders, or DSM-IV.
PMDD, which is thought to affect fewer than 5 percent of menstruating women, is described by the
APA as a pattern of severe, recurrent symptoms of depression and other negative moods that occur
during the last week of the menstrual cycle and markedly interfere with daily living. While PMDD is
not an official diagnostic category, the APA hopes its inclusion in DSM-IV will encourage further
psychiatric research into the condition. (See "Spelling out PMDD.")
Sugar can also play havoc on your body, especially in the days preceding your period. Eating sugary foods often initiates a vicious
cycle of additional sugar cravings, as an increase in your body's need for B-complex vitamins prompts even more craving for sugar-
laden simple carbohydrates. Although a link between PMS and difficulties in metabolizing sugar has not been proven, consuming
sweets can put your body on a roller coaster between feeling weak and feeling high strung and jittery—your body's response to low
sugar levels at one extreme, and elevated sugar levels at the other.
Nicotine, a brain stimulant, can magnify PMS symptoms much like caffeine, so reducing or eliminating smoking should be part of any
treatment program. Alcohol can also intensify symptoms because it depletes the body of B vitamins, disrupts the metabolism of
carbohydrates, and affects the liver's ability to process hormones.
Some foods may genuinely relieve PMS symptoms. Complex carbohydrates such as whole grains, beans, fresh fruits, and vegetables
help to maintain your body's essential vitamins and minerals. Eating a low-fat diet based on grains and vegetables while reducing your
intake of red meat—especially during the two weeks prior to the beginning of your period—may help to control your PMS symptoms.
And at least one study has suggested that taking a supplementary 1,200 milligrams of calcium per day reduces many PMS symptoms,
including irritability, water retention, food cravings, and pain.
Many women also find that exercise produces positive benefits in moderating PMS symptoms, while improving their general health.
Consider a monthly workout plan that rotates activities designed to strengthen your muscles, reduce fat, and relieve tension. Vigorous
exercise—running, biking, swimming, aerobics, racquet sports and the like—has been shown to elevate your mood and improve
alertness, while calisthenics and body-building tone muscles and improve strength. Contrary to popular belief, exercise helps to
control—not increase—your appetite.
With your doctor's approval, try a program that mixes more vigorous cardiovascular exercises during the early days of your menstrual
cycle with stretching, flexibility exercises, and less vigorous cardiovascular work such as walking on the days when you're most prone
to PMS symptoms. This regimen can increase your heart-lung capacity and improve your overall physical condition while reducing the
strain on your breasts, thighs, and abdomen during the latter phase of your cycle.
PMS is also associated with disruptions in a woman's normal sleep patterns. Women with moderate to severe PMS symptoms are more
likely to complain of insomnia and are known to spend less time in deep sleep than those who are symptom-free. Reducing caffeine
intake can help. You may also benefit from short naps on certain days. In any event, try to get at least eight hours of uninterrupted
sleep each night, especially during the latter half of your cycle.
You may also benefit from some stress management techniques. Unlike diet, exercise, and sleep, outside stress is the one factor of
daily life that no one can control. How you approach and handle stress, however, can have a tremendous impact on your behavior and
mood.
The causes of stress can be physical, such as chronic or episodic illness or injury; psychological, such as fears, anxieties, or
frustrations; and social, such as crying children, rush-hour traffic, and even holiday preparations. These everyday aggravations are
particularly annoying during the days you're experiencing PMS symptoms.
A stress management class can help you channel the tension caused by stress so you are less likely to lose control, a common
complaint of women with PMS. Whether they emphasize breathing exercises, visualization, biofeedback, or other stress management
techniques, a common theme is to help you maintain a positive attitude and develop realistic expectations.
How much improvement you can expect from these remedies—and how quickly—depends largely on your commitment to them and
your willingness to change your habits. You may notice dramatic improvements almost immediately, or gradual improvement over
several menstrual cycles. As you continue to record your symptoms, you may observe that more sleep or a brisk walk helps during
certain premenstrual days, while modifying your diet helps during others. The bottom line is to focus on continual improvement rather
than dwell on the symptoms.
Even though you can make many of these lifestyle and dietary changes without seeing a physician, it's better to enlist your doctor's
expertise in developing a program tailored to your particular PMS symptoms and other health factors. Since no single treatment is
uniformly effective for PMS, you can benefit from your physician's experience with other women who are successfully managing their
condition.
Available Medical Treatments
Lifestyle and dietary changes generally provide some degree of relief to all women who experience PMS-related distress. If your
condition improves only modestly, however, your doctor may suggest a medical approach. Since there are many claims made for the
benefits offered by vitamins, food supplements, and some over-the-counter medications, you should not use any of them without
consulting your physician. It is important to remember that while some physicians support the use of certain vitamins and
supplements and believe in their possible effectiveness, others cite the lack of scientific evidence of any benefit, and warn of possible
harm if the products are consumed in large doses. Among the many "PMS formulas" on the market are a number of multivitamins
containing some combination of vitamin B
6
, magnesium, zinc, and vitamin A. The use of vitamin B
6
for PMS dates back to the 1940s.
For those who believe in its effectiveness, the connection is thought to be in the vitamin's interaction with certain brain chemicals.
However, its effectiveness has not been clinically proven and large amounts have been shown to be harmful. As little as 200 to 300
milligrams a day has been reported to cause toxic reactions resulting in pain or numbness in the hands or feet, awkwardness in
walking or general clumsiness and nerve damage.
Some physicians have claimed that the dietary supplement oil of evening primrose, which contains linoleic acid and gamma-linoleic
acid, helps relieve breast tenderness. However, while it's true that evening primrose oil has an anti-inflammatory effect, there is no
conclusive evidence that it helps in PMS.
The benefits of some vitamins and food supplements, though still unproven, seem a bit more promising. In one study, vitamin E in
dosages of 150 to 300 milligrams daily was reported to reduce PMS symptoms. Another study suggested that a daily 200 milligram
magnesium supplement may counter some of the physical and behavioral changes associated with PMS, though magnesium can also
be toxic in high doses and can impair calcium absorption. Finally, the amino acid L-tryptophan, banned from over-the-counter sales
but available by prescription from a few qualified pharmacies, has seemed to help some women. It may raise the serotonin level,
allowing for a more restful sleep and reducing restlessness and food cravings.
Your physician may also choose from an array of prescription medications, though no "PMS drug" has yet been developed, and the
effectiveness of pharmaceuticals in treating PMS has generated considerable debate. In fact, some of the medications used for PMS
are potentially harmful, so you and your doctor should plan a conservative course of symptom management rather than generalized
drug therapy.
Diuretics, or "water pills," help the body eliminate excess fluid through the kidneys. Your doctor may prescribe a diuretic to reduce
bloating if restricting your salt intake does not help. Although studies on the benefits of diuretics for PMS have shown mixed results,
they have been used longer in PMS treatment than any other medication, and have been shown to ease other symptoms, such as
fatigue and depression.
Because it inhibits the action of the hormone that causes water retention, spironolactone (Aldactone) is also selected to treat PMS
symptoms. Physicians typically prescribe 25 milligrams of spironolactone four times a day from the time of ovulation to the onset of
menstruation.
Bromocriptine, a drug that suppresses lactation after childbirth, is sometimes used to reduce PMS-related breast discomfort, though
there is no evidence that women taking this medication show greater improvement than those who don't. The usual dosage is 2.5
milligrams once or twice daily from the date of ovulation until your period begins. Because there is a risk of side effects, your doctor
will probably start this drug cautiously at low doses.
Mefenamic acid (Ponstel) is a non-steroidal, anti-inflammatory drug that is sometimes used to relieve premenstrual pain. The usual
starting dose is 500 milligrams when symptoms appear, followed by 250 milligrams twice a day for two to three days. A major risk
with this medication is its uncertain effect on a developing baby. Since PMS follows ovulation, you may not know you are pregnant
until your period is late. Therefore, your physician may advise you to use a barrier contraceptive before prescribing mefenamic acid or
other medications used to treat PMS symptoms. A variety of nonsterodial anti-inflammatory drugs are available, including such over-
the-counter products as ibuprofen (Advil, Motrin IB) and naproxen (Aleve). However, all carry a risk of stomach inflammation with
habitual use. Other over-the-counter remedies, such as Midol and Women's Tylenol, promise relief from cramps, bloating, and pain
without harm to the stomach.
Progesterone therapy has also gained many advocates, despite the fact that neither natural progesterone nor synthetic progestins has
been shown to be effective in scientific studies. In fact, the use of progesterone to treat PMS has not been approved by the FDA, and
some scientists question the long-term safety and consequences of this therapy. Nevertheless, because some physicians claim to have
seen improvements in their own patients, the use of progesterone to treat PMS symptoms remains common. According to the
American College of Obstetricians and Gynecologists, the standard dosage for treating PMS is 50 to 100 milligrams of progesterone
administered daily by intramuscular injections or 200 to 400 milligrams twice a day by vaginal or rectal suppositories. Treatment is
started several days before symptoms are expected and is continued through the onset of a woman's period.
Spelling Out PMDD
Listed below are the official criteria for a diagnosis of "premenstrual depression." "Luteal phase" refers to the second half of the
menstrual cycle, following release of an egg. "Follicular phase" refers to the first half of the cycle. "Dysphoric" is medical jargon
meaning "unhappy."
Criteria for Late Luteal Phase Dysphoric Disorder
A. In most menstrual cycles during the past year, symptoms in B occurred during the last week of the luteal phase and remitted
within a few days after onset of the follicular phase. In menstruating females, these phases correspond to the week before, and
a few days after, the onset of menses. (In nonmenstruating females who had a hysterectomy, the timing of luteal and follicular
phases may require measurement of circulating reproductive hormones.)
B. At least 5 of the following symptoms have been present for most of the time during each symptomatic late luteal phase, at least
one of the symptoms being 1, 2, 3 or 4:
1. Marked affective lability, e.g., feeling suddenly sad, tearful, irritable, or angry.
2. Persistent and marked anger or irritability.
3. Marked anxiety, tension, feelings of being "keyed up" or "on edge."
4. Markedly depressed mood, feelings of hopelessness, or self-deprecating thoughts.
5. Decreased interest in usual activities, e.g., work, friends, hobbies.
6. Easy fatigability or marked lack of energy.
7. Subjective sense of difficulty in concentrating.
8. Marked change in appetite, overeating, or specific food cravings.
9. Hypersomnia or insomnia.
10. Other physical symptoms, such as breast tenderness or swelling, headaches, joint or muscle pain, a sensation of "bloating,"
weight gain.
C. The disturbance seriously interferes with work or with usual social activities or relationships with others.
D. The disturbance is not merely an exacerbation of the symptoms of another disorder, such as major depression, panic disorder,
dysthymia (chronic mild depression), or a personality disorder (although it may be superimposed on any of these disorders).
E. Criteria A, B, C, and D are confirmed by prospective daily self-ratings during at least two symptomatic cycles. (This diagnosis
may be made provisionally prior to this confirmation.)
Source:
American Psychiatric Association, Washington, DC.
A few studies indicate that medicines used to block ovarian function, known as "medical ovariectomy," can halt the symptoms of PMS.
In clinical trials, this has been accomplished by using Lupron as an injection or Synarel as a nasal spray to block the action of GnRH,
the hormone that starts the menstrual cycle with stimulation of the ovaries.
However, blocking ovarian function essentially creates an artificial menopause, which can lead to osteoporosis and other
postmenopausal medical problems. As a result, this approach is considered only in severe and disabling cases of PMS: the 5 to 10
percent of women whose PMS symptoms cause incapacitating disruptions to their jobs or family life. Therapy is generally discontinued
after six months.
Some physicians prescribe tranquilizers or antidepressants, including fluoxetine hydrochloride (Prozac) for patients diagnosed with
PMS. However, unless you suffer from the depressive effects of PMDD, such drugs are probably not justified. They can cause serious,
even fatal, reactions in combination with other drugs and can lead to a wide range of side effects. They are generally reserved for
serious illnesses such as major depression.
On the other hand, if you have been diagnosed with PMDD, the doctor may prescribe a version of Prozac called Sarafem. This
antidepressant has proven effective when taken in doses of 20 milligrams a day throughout the entire menstrual cycle. The most
common side effects are headache, nausea, and runny nose.
Other Treatment Approaches
Nontraditional approaches to PMS treatment, such as acupuncture, chiropractic adjustment, therapeutic massage, and over-the-
counter "natural" progesterone creams have, in the past, been ignored by the medical community although this is slowly changing.
Some women experience symptom relief, although no studies have documented the safety or effectiveness of nontraditional
approaches and any benefits are considered speculative.
On the other hand, many women unquestionably benefit from joining a PMS support group. This can be particularly helpful when you
are trying to modify certain behaviors, such as dietary habits. Meeting and talking with other women who share the condition, and
having access to current PMS research are important benefits of support groups, as are the empathy and reassurance.
It's also possible that even the most classic cycle of PMS symptoms is masking an unrelated psychological or psychiatric problem. A
skilled therapist can help uncover the presence of any hidden conditions. In general, psychotherapy can also help a woman explore
the specific emotional issues that affect her premenstrually and learn healthy ways to express anger and frustration—common
manifestations of PMS.
In any event, it's important to collaborate with your doctor while finding a treatment that works for you. Remember that even with
your doctor's help, you may have to try several different approaches before you find relief. Keep charting your symptoms and
remember that no single treatment for PMS is a one-step or permanent cure. If after a month or two of treatment, there is no change
in your symptoms, you and your doctor can modify your action plan.
Taking Control
If left undiagnosed or untreated, PMS can have a major impact on a woman's life. Whether at home or on the job, you may have to
struggle to function normally when symptoms occur. Emotional distress caused by PMS may trigger marital or family conflicts. You
may feel an increased desire for intimacy with your partner yet feel sexually unattractive. You may even notice that PMS prompts you
to withdraw socially.
Recognizing these changes in your body and mood and planning strategies to accomodate them is half the battle. The more you
understand yourself and your monthly menstrual cycle, the better you can manage your PMS symptoms.
Follow your treatment program faithfully and learn to communicate your feelings with others. On the days you feel most anxious or
tired, enlist the help of family members to prepare meals or run errands so you can reduce the pressure on yourself. While the goal of
PMS management is to maintain a normal lifestyle even during your most difficult days, don't create needlessly difficult targets for
yourself by adopting the standards of a superhero.
Many women find that there are days when PMS interferes with productivity or relationships at work. Though some physicians still
advocate avoiding or postponing extra tasks on days when PMS symptoms are the most challenging, many women find that taking
charge of their health and moving forward with planned schedules and tasks helps them get through their PMS symptoms. As you
undertake some of the strategies outlined here and reduce the overall impact of PMS on your life, you may discover that your job, too,
seems more manageable.
Although much work remains to be done before PMS is fully understood, the good news is that millions of women successfully manage
their homes, jobs, academic pursuits, and creative endeavors at every phase of their menstrual cycle. Until the cause of PMS is finally
established and a standardized treatment is developed, your best tactic is to understand your own PMS symptoms and take the
initiative to control them.
Source: From the PDR® Family Guide to Women's Health and Prescription Drugs™