Uterine Health
Treatment Options That Help
You Take Charge Again
What We’ll Talk About Today
I. The Female Reproductive System
II. Uterine Conditions & Treatment Options
-Menorrhagia
-Fibroids
III. Hysterectomy
-Laparoscopic Supracervical Hysterectomy
IV. Questions & Resources
Uterine Health and You
• Reproductive functions change as you move
through life
• Hormone imbalances, infection and disease
can affect the function of your uterus
• This presentation will discuss fibroids and
heavy periods, common in women in their 30s
and 40s
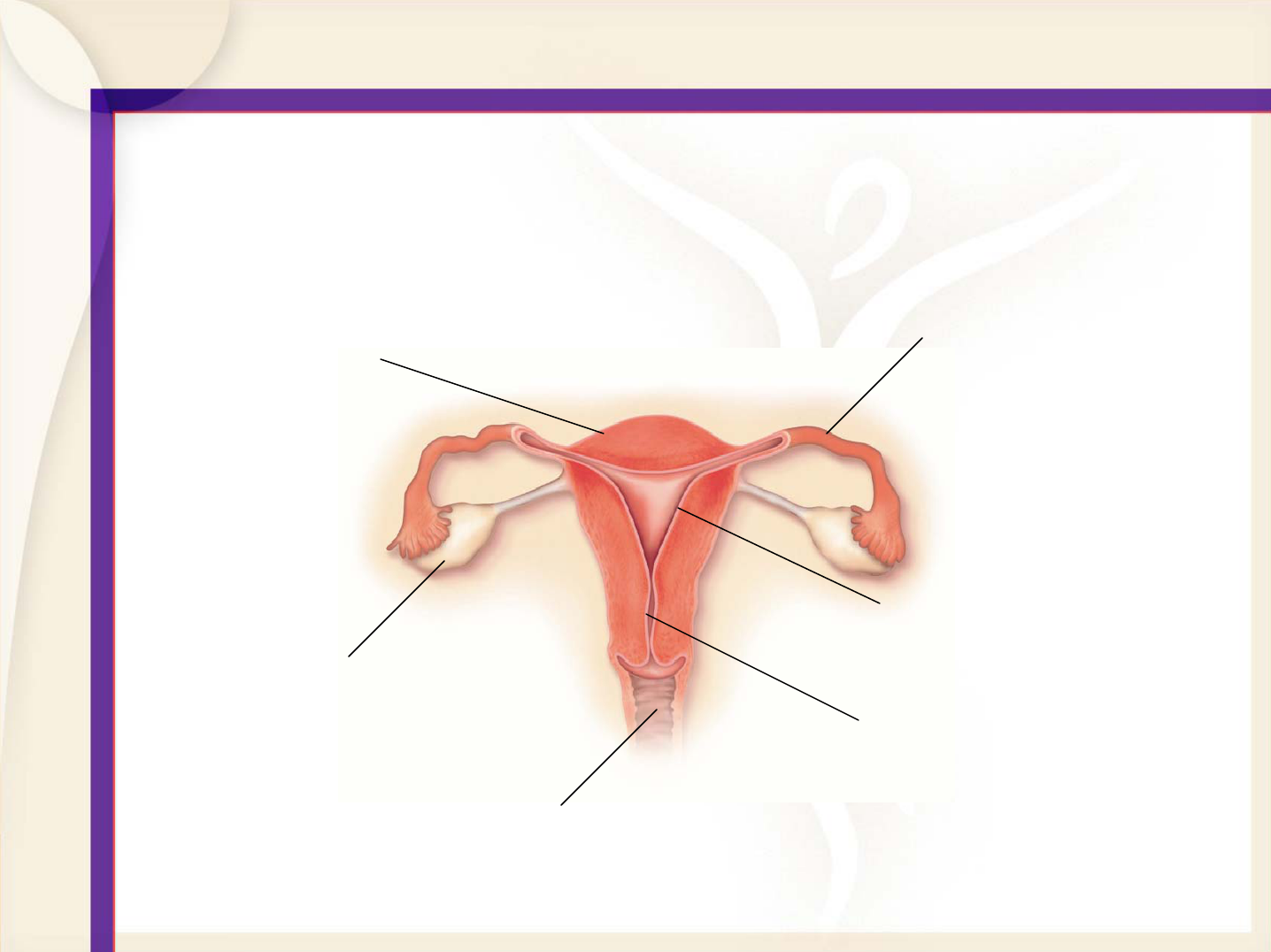
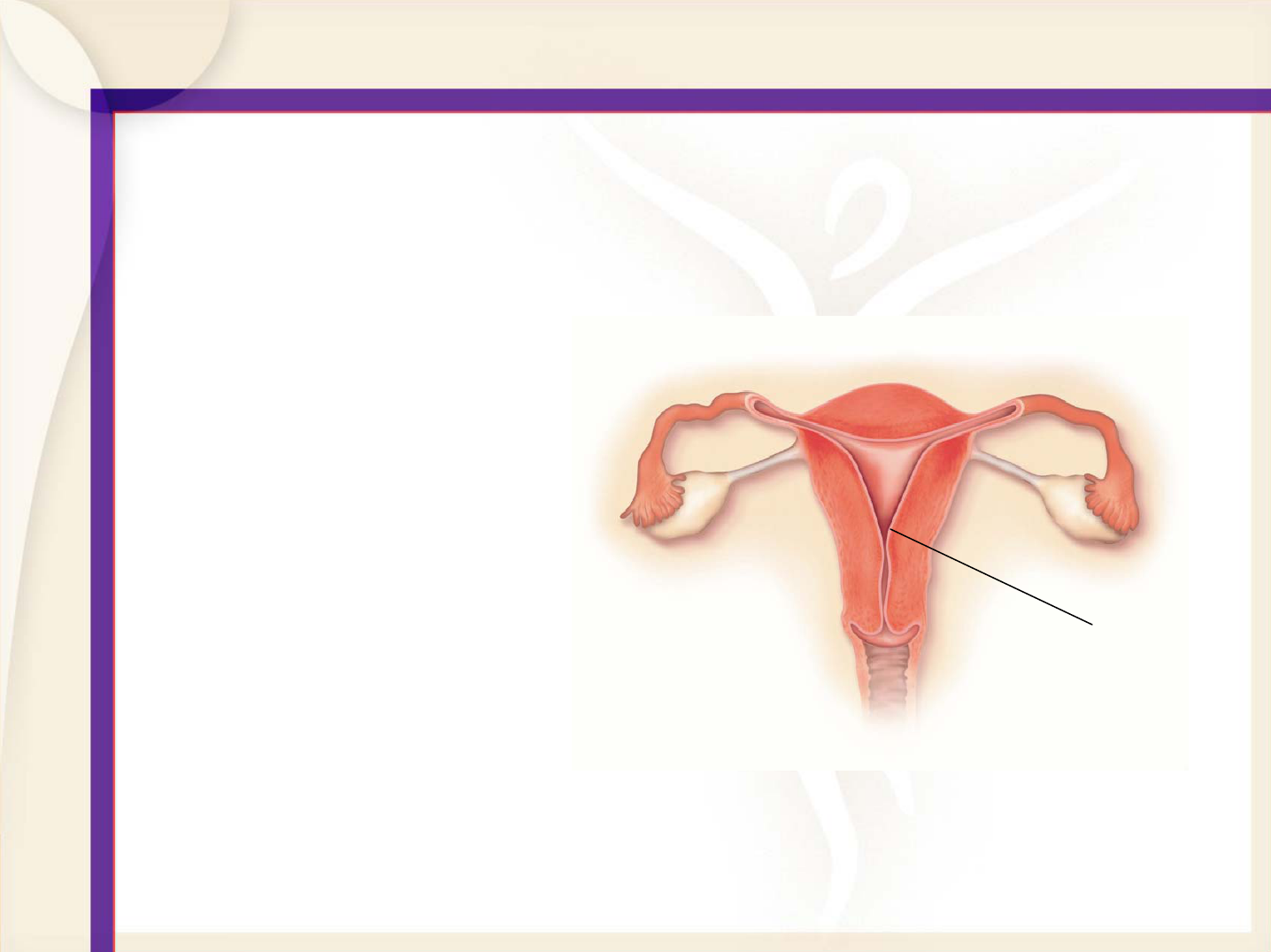
Overview of Reproductive System
Uterus
Ovaries
Endometrium
Fallopian tubes
Cervix
Vagina
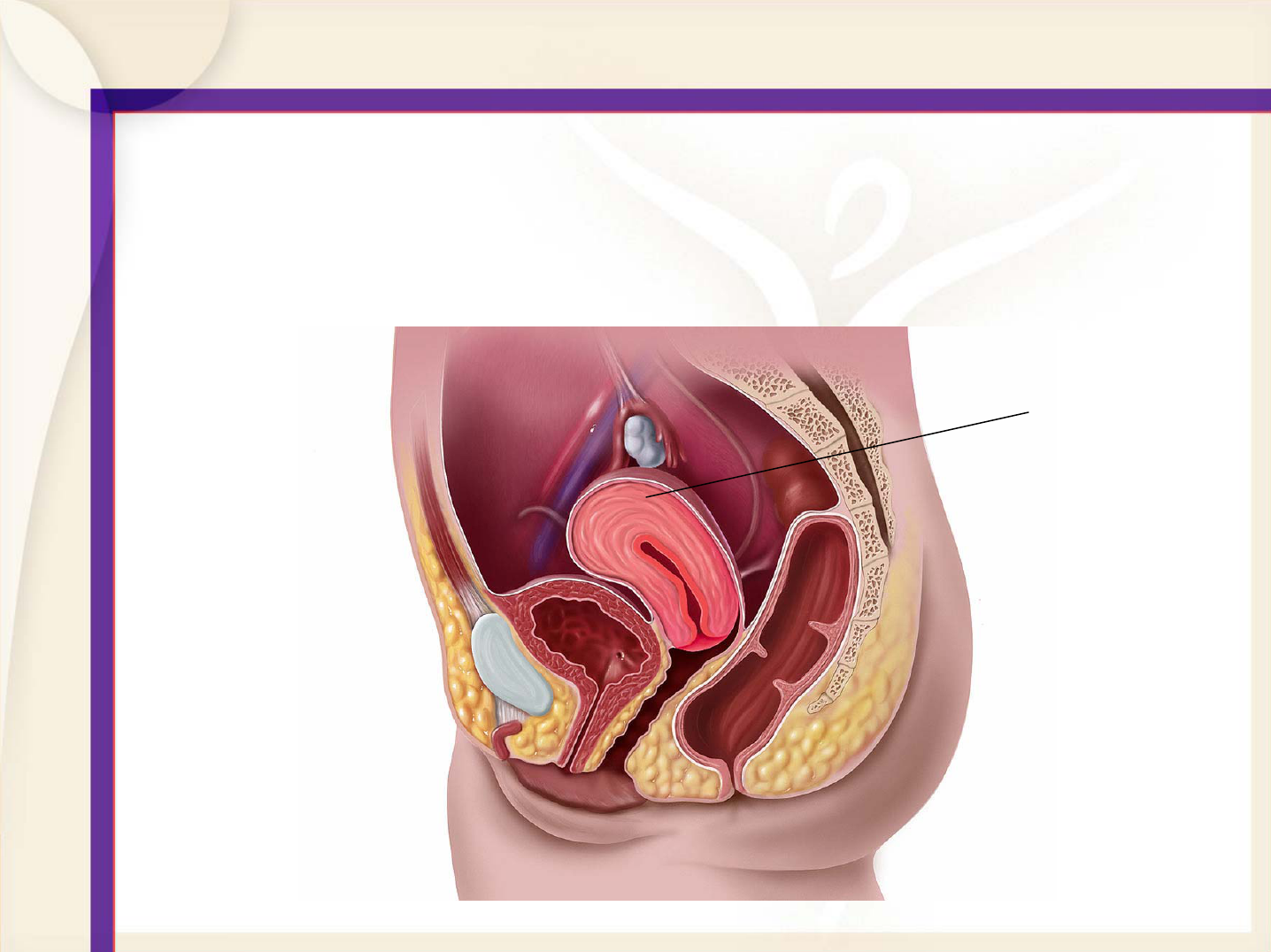
Female Anatomy
Uterus
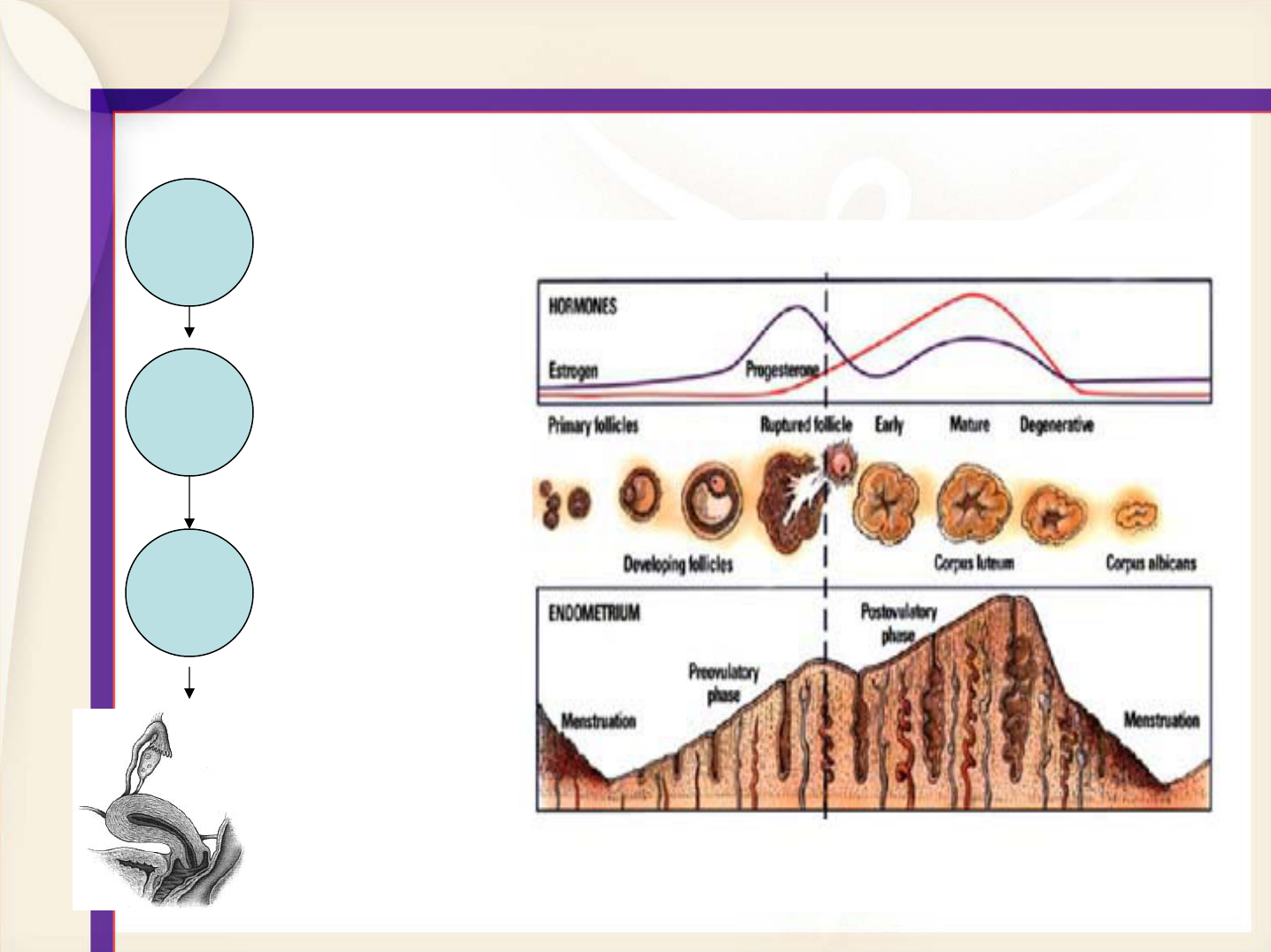
The Menstrual Cycle
Hypothalamus
Pituitary
Ovarian
Uterus
Heavy Periods
and Treatment
Options
What is Excessive Menstrual
Bleeding?
• Unmanageable or
heavy bleeding month
after month
• Also known as
menorrhagia
(men-or-ah-zha)
•1 out of 5 women have heavy periods
For some women, this means:
• Bleeding for more than 7 days
• Using more than 10 pads or
tampons per day during a
period
• Feeling tired, worrying about
embarrassing accidents and
generally feeling frustrated
that periods rule one’s quality
of life
Changes in Your Menstrual Cycle
• Many women experience a change in their
periods six or more years leading up to
menopause – commonly referred to as
perimenopause
• Typically, women in their 30’s and 40’s may
experience heavier periods
• Some women always have heavy periods
What Causes Heavy Bleeding?
• Hormonal imbalance
• Fibroids (benign
uterine growths)
• Infection/Disease
How is Heavy Bleeding Diagnosed?
• Pelvic Exam
• Ultrasound
• Hysteroscopy
• Endometrial Biopsy
Hormonally-Caused Heavy Bleeding
and
Treatment Options
Medication
• Birth control pills may be prescribed to
control heavy bleeding
• Drawbacks:
• Not always well tolerated
• Not always effective
• May have to be taken until menopause
Endometrial Ablation
• Removes uterine
lining and
preserves the
uterus
• Performed under
general or local
anesthesia
• Option for women
past childbearing
Endometrial
lining
GYNECARE THERMACHOICE*
Uterine Balloon Therapy
• Can be performed under local anesthesia
• Simple outpatient treatment, no incision
required
• Treats endometrium, preserves uterus
*Trademark of ETHICON, Inc.
How It Works
•Uses hot liquid in balloon to treat uterine lining
•Minimally invasive, inserted through cervix
•Procedure is quick, uterine lining is treated for 8 minutes
•Uterine lining will slough off like a period in 7-10 days
Benefits of
GYNECARE THERMACHOICE
• 95% of patients report normal bleeding
levels or less*, 93% patient satisfaction
• Clinical data shows that women who have
menorrhagia and have undergone treatment
with Thermachoice experienced a decrease
in painful periods
• Non-hormonal, one-time treatment
Drawbacks of
GYNECARE THERMACHOICE
• Rare side effects include blood loss, heat
burn of internal organs, perforation or
rupture of uterine wall, leakage of heated
fluid into cervix or vagina
• All medical procedures have potential risks
Who is a Candidate?
• Pre-menopausal woman
• Childbearing complete
• Normal pap smear and
biopsy
Patient Testimonial
“There were two days out of every
month that I knew that I wasn’t going
to be able to leave the house and I
would have to reschedule
appointments or just totally miss
work. It’s great now. I really don’t
have to plan around my menstrual
cycle. I know what I’m in for
basically and it’s not at all what it use
to be so I’m very glad I got the
THERMACHOICE treatment done.”
Debby
Fibroids
And Treatment Options
Fibroids
• May cause heavy bleeding, pain, infertility
• Occurs in 20% of pre-menopausal women
• Exact cause is unknown, but evidence
suggests that many fibroids require
estrogen to grow
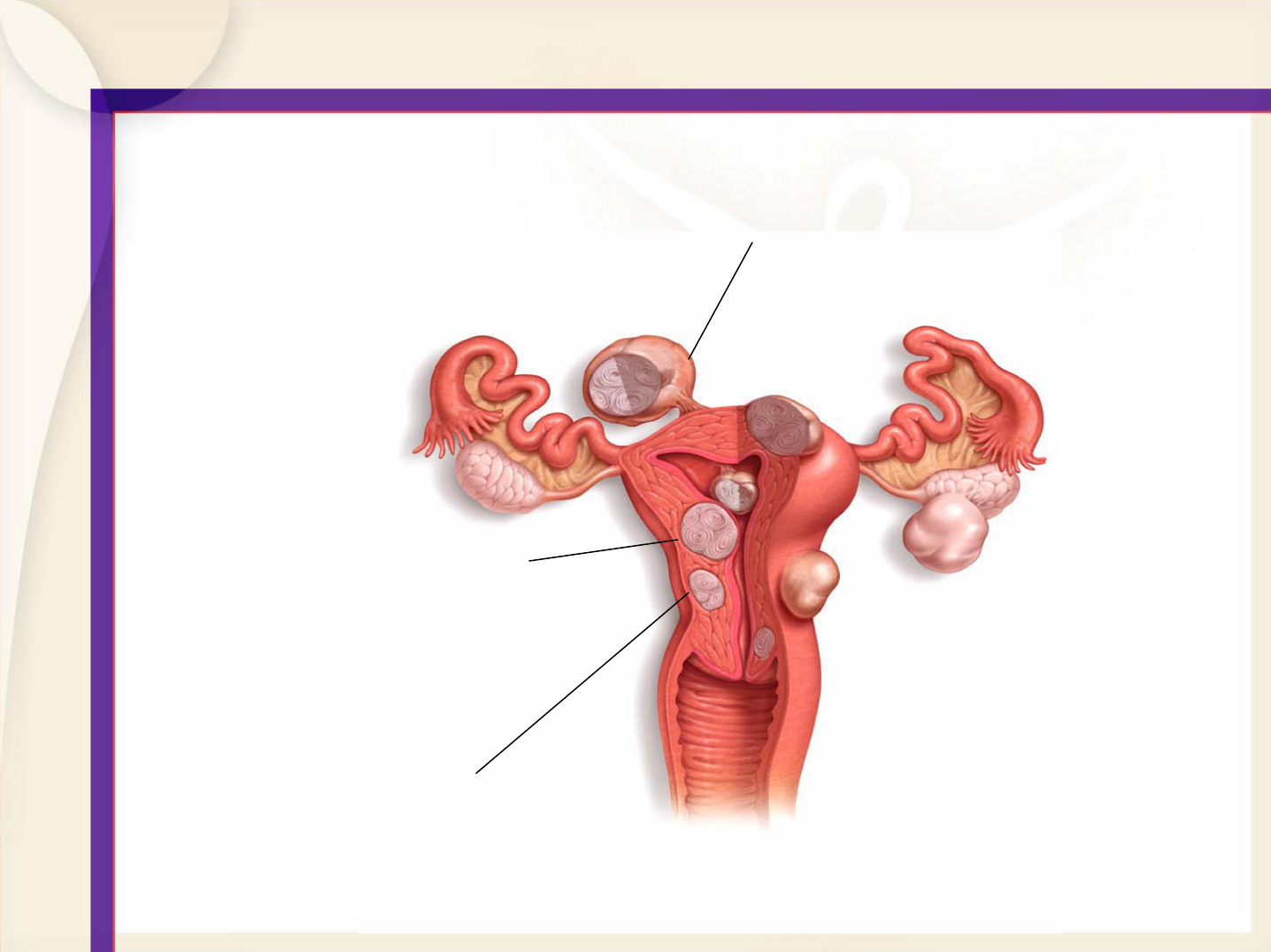
Types of Fibroids
Intramural:
occurs within
uterine wall
Submucosal:
grows into
uterine cavity
Pendunculated
subserosal: grows
from uterine wall to the
outside uterine cavity
• Pelvic exam
• Ultrasound
• Hysteroscopy
• Laparoscopy
How are Fibroids diagnosed?
Medication
• Typically used to shrink fibroids before
surgical removal
• Fibroids may return soon after
discontinuation of treatment
• May produce menopause symptoms
Fibroid Removal – Surgical Options
• Myomectomy
• Embolization: A non-surgical option
Myomectomy
• Removes just
fibroids, preserving
uterus
• Women may still be
able to have children
• Types:
• Open
• Laparoscopic
• Hysteroscopic
Benefits of Hysteroscopic and
Laparoscopic Myomectomy
• Can maintain fertility, preserves the uterus
• Option to avoid major surgical procedures
• Outpatient procedure, no hospital stay
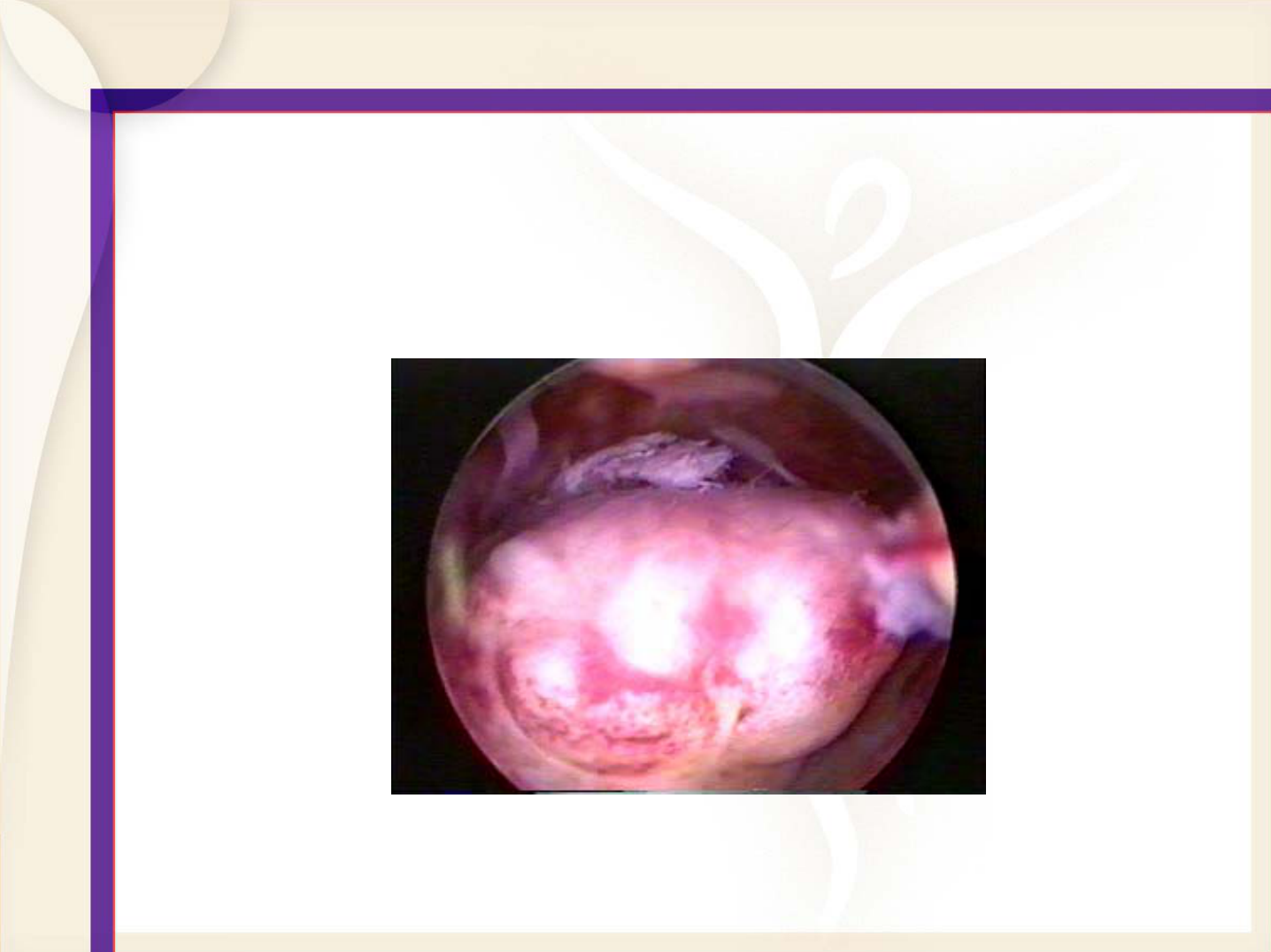
Hysteroscopic Myomectomy
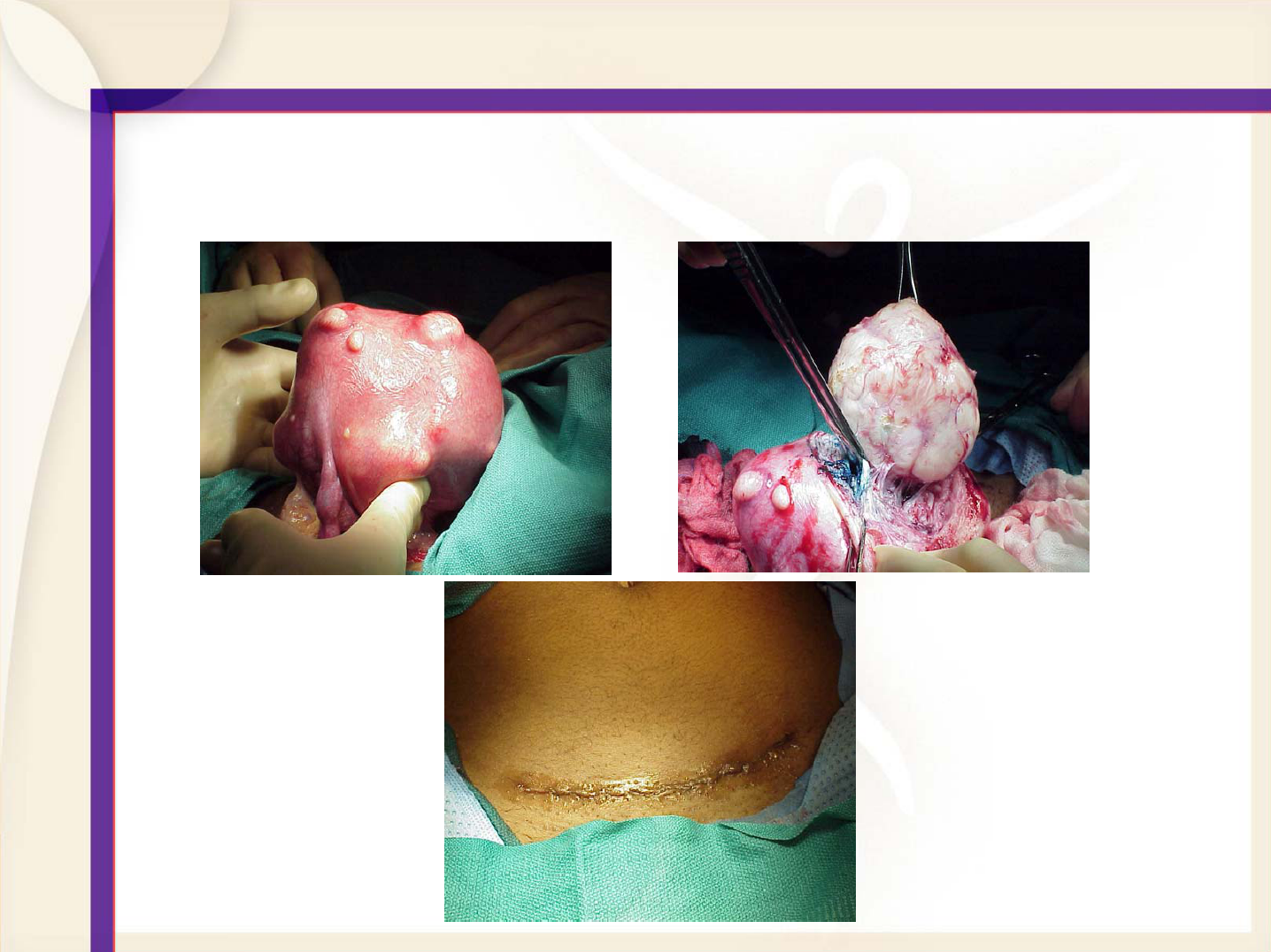
Abdominal Myomectomy
Drawbacks of Myomectomy
• Fibroids may come back after surgery, and
repeat surgery may be necessary.
• Other potential risks include:
• Bleeding, infection, damage to vital organs
• May result in perforation to uterus
Fibroid Embolization
• Blocks blood supply to fibroids causing
them to shrink
• Appears effective, long-term results
unknown
• Not recommended for women planning to
have children
Hysterectomy
Hysterectomy
• Surgical removal of uterus
• May or may not remove the fallopian tubes and
ovaries
• Should only be considered after other
options have been explored
• Major surgery, usually requires hospital
stay
Is It Necessary?
• In most cases, hysterectomies are elective
procedures
• Know your options:
Different ways to perform hysterectomy
Abdominal Hysterectomy
• Major surgery; most invasive
type of hysterectomy
• Removes uterus and cervix
through abdominal incision
• Performed under general
anesthesia
• Requires hospital stay of
3-6 days, long recovery period
(up to 6 weeks).
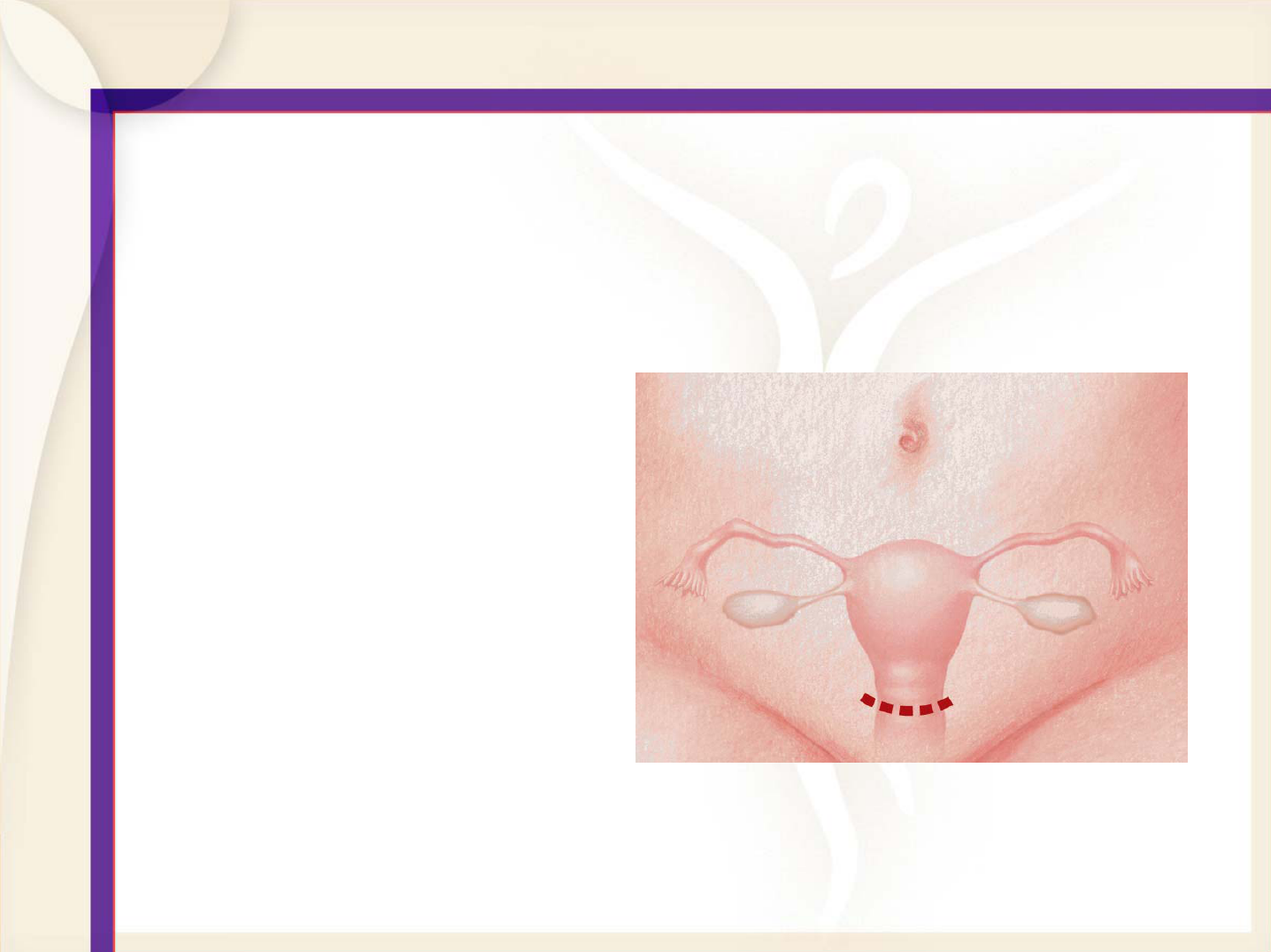
Vaginal Hysterectomy
• Removes uterus
and cervix through
incision inside
vagina
• Typical hospital
stay, 1-3 days
• Average recovery
time, 4 weeks
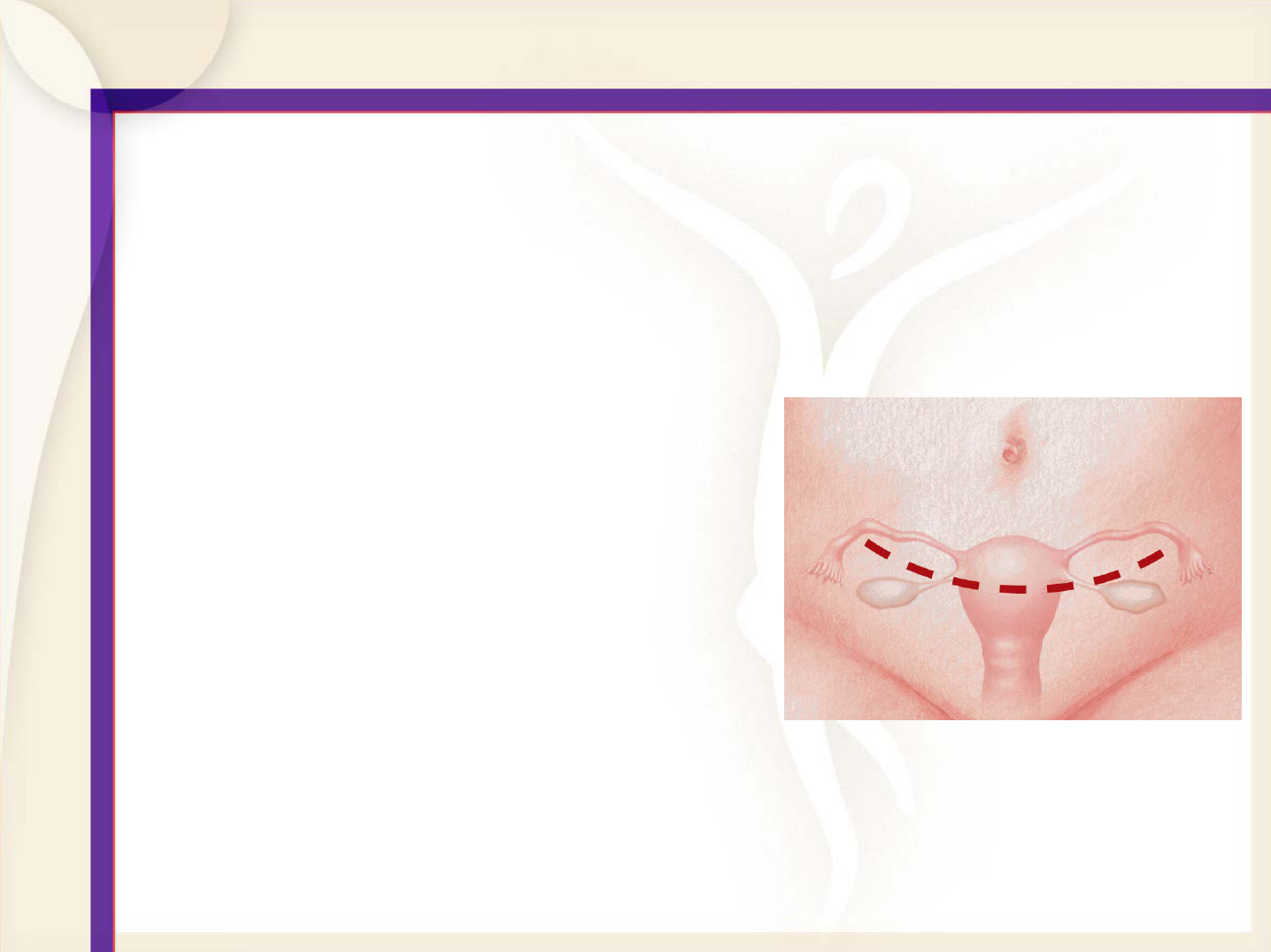
Laparoscopic-assisted Vaginal
Hysterectomy (LAVH)
• Removes uterus
and cervix
• Laparoscope
inserted through
small incision in
navel
• Typical hospital
stay, 1-3 days
• Average recovery
time, 4 weeks
Not Your Mother’s Hysterectomy
Laparoscopic Supracervical Hysterectomy
An innovative approach
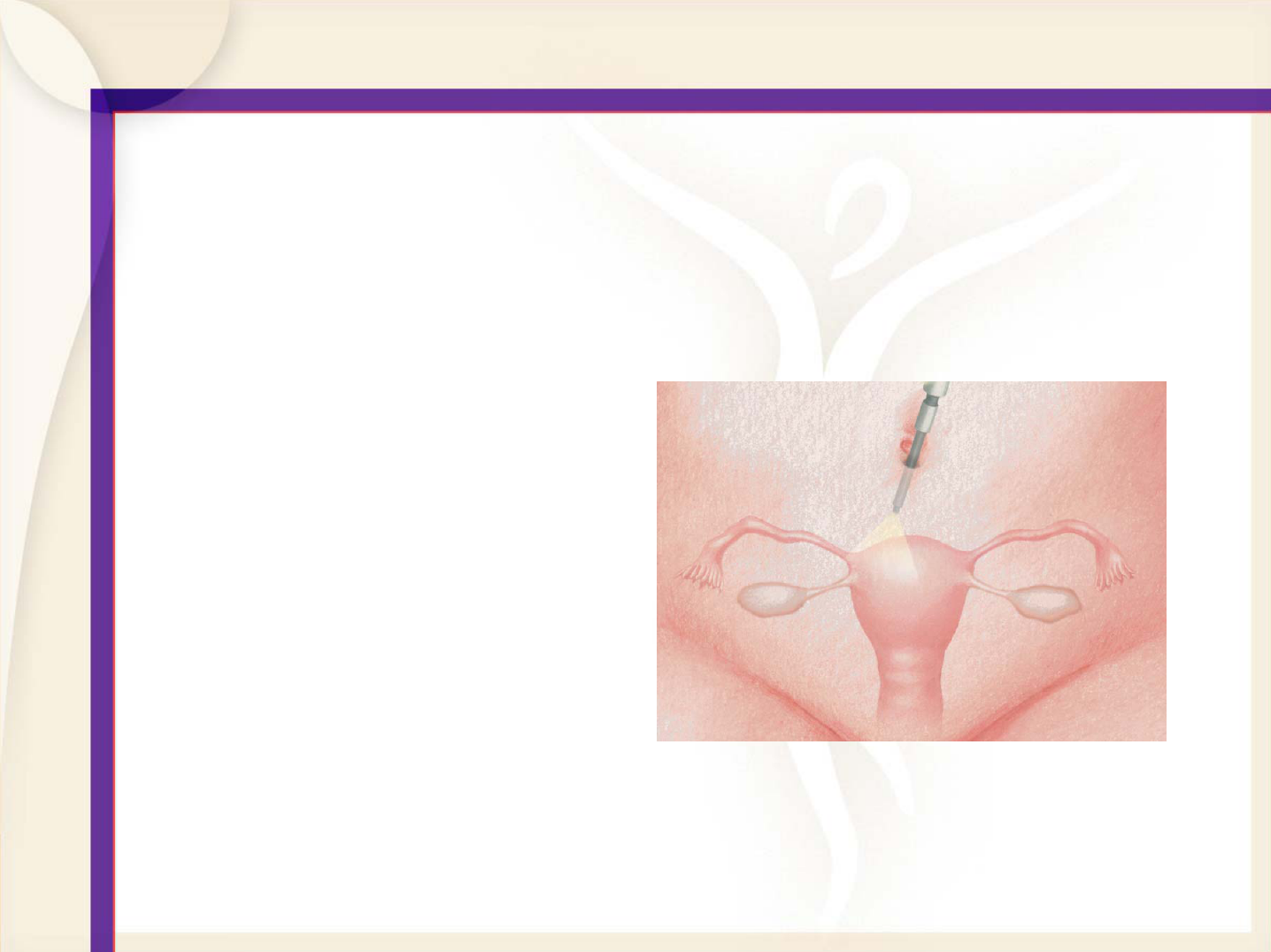
Laparoscopic Supracervical
Hysterectomy
Using laparoscopy:
(small abdominal incisions)
• Detach and removes top
part only of the uterus
• Leaves cervix (lower
portion) in place
• Considered a partial
hysterectomy
LSH
Benefits:
• Typical hospital stay, one day or less
• Average recovery time, six days
• Less invasive, minimal scarring
• Less traumatic for your body
LSH
Why should I consider preserving my cervix?
May help reduce complications
associated with total hysterectomies,
such as pelvic floor prolapse and
urinary incontinence
LSH
Is there any downside to retaining my cervix?
You will need to continue regular pap
test to screen for cervical cancer and
you may still have slight bleeding every
month
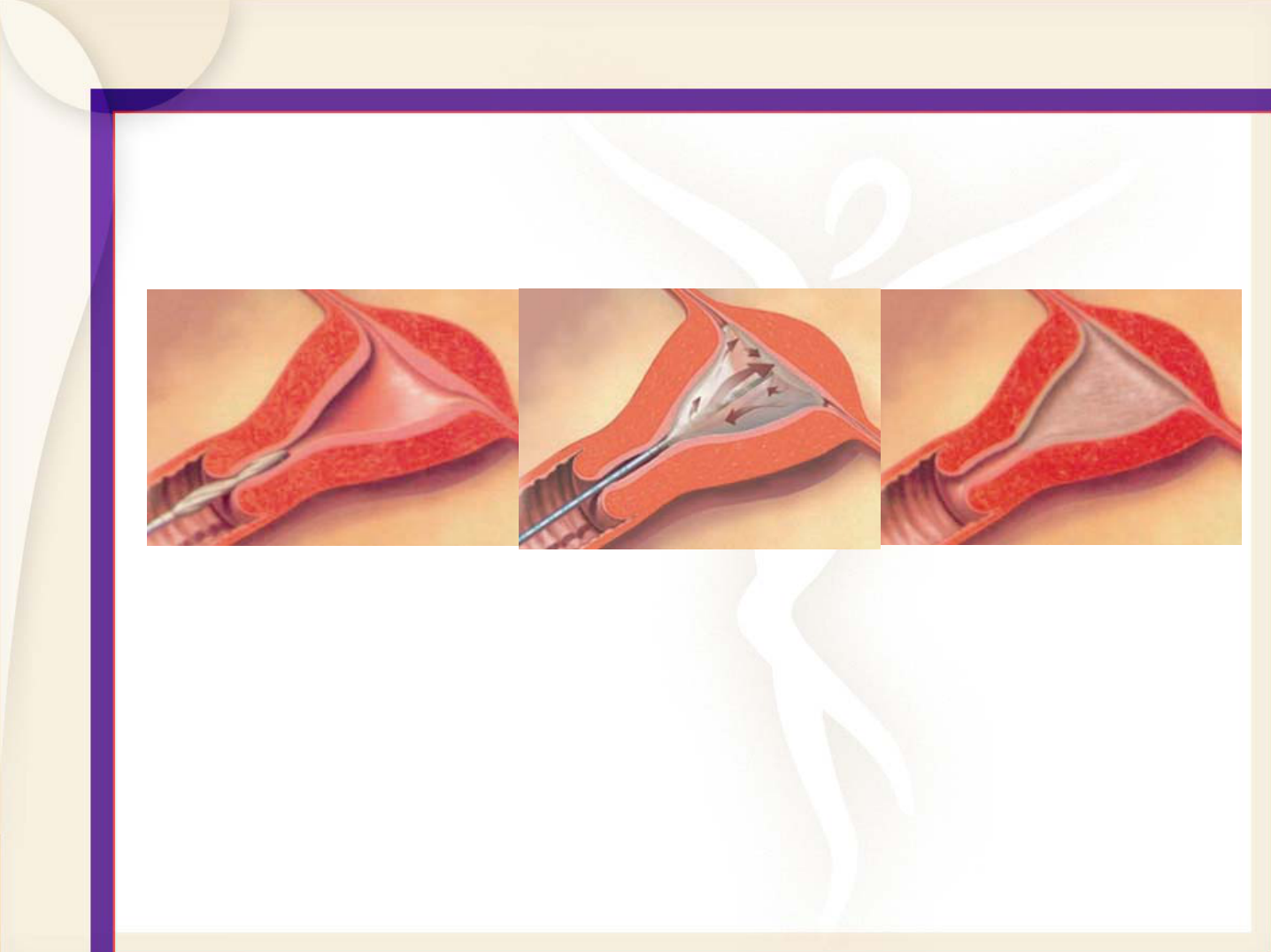
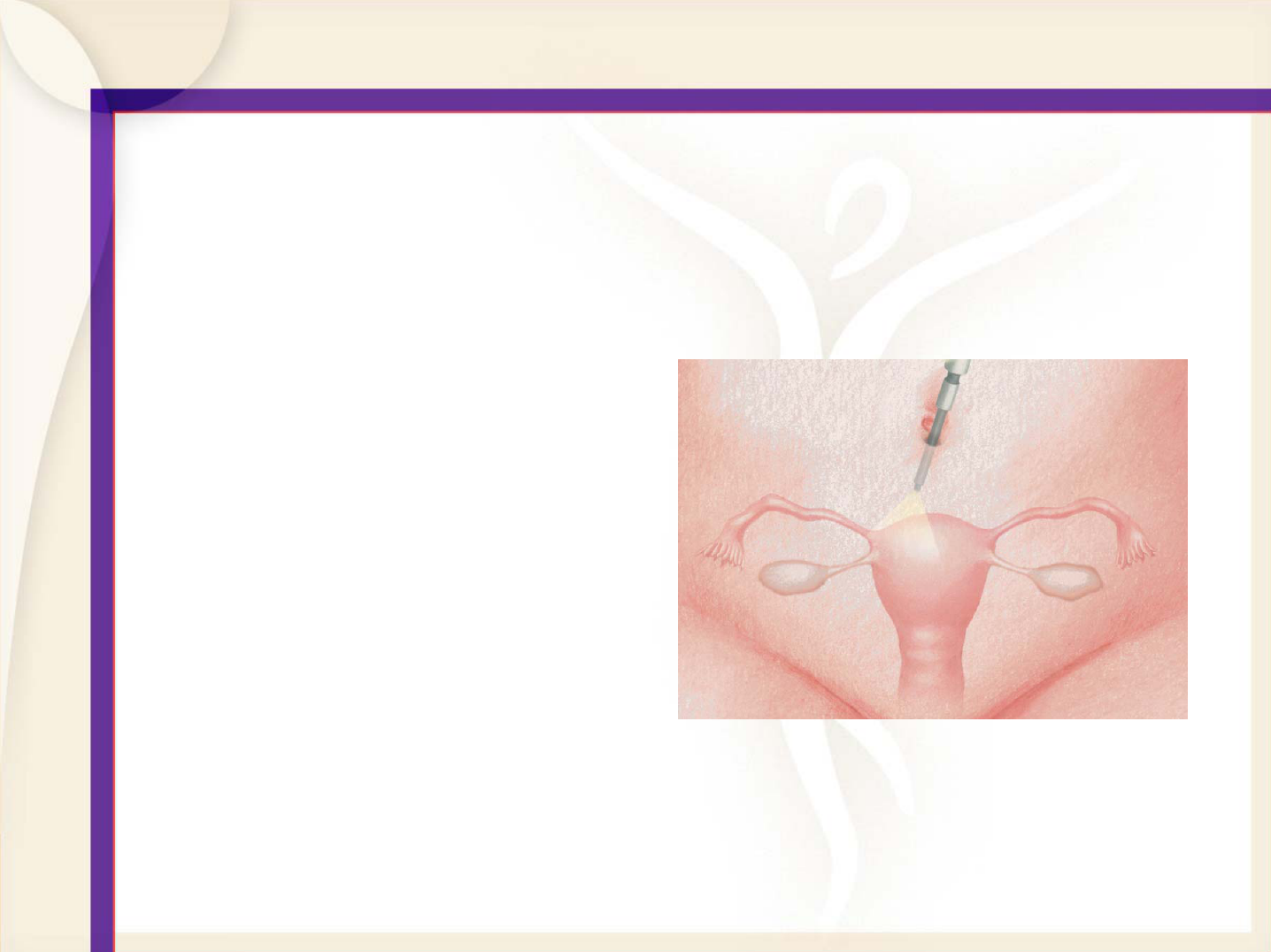
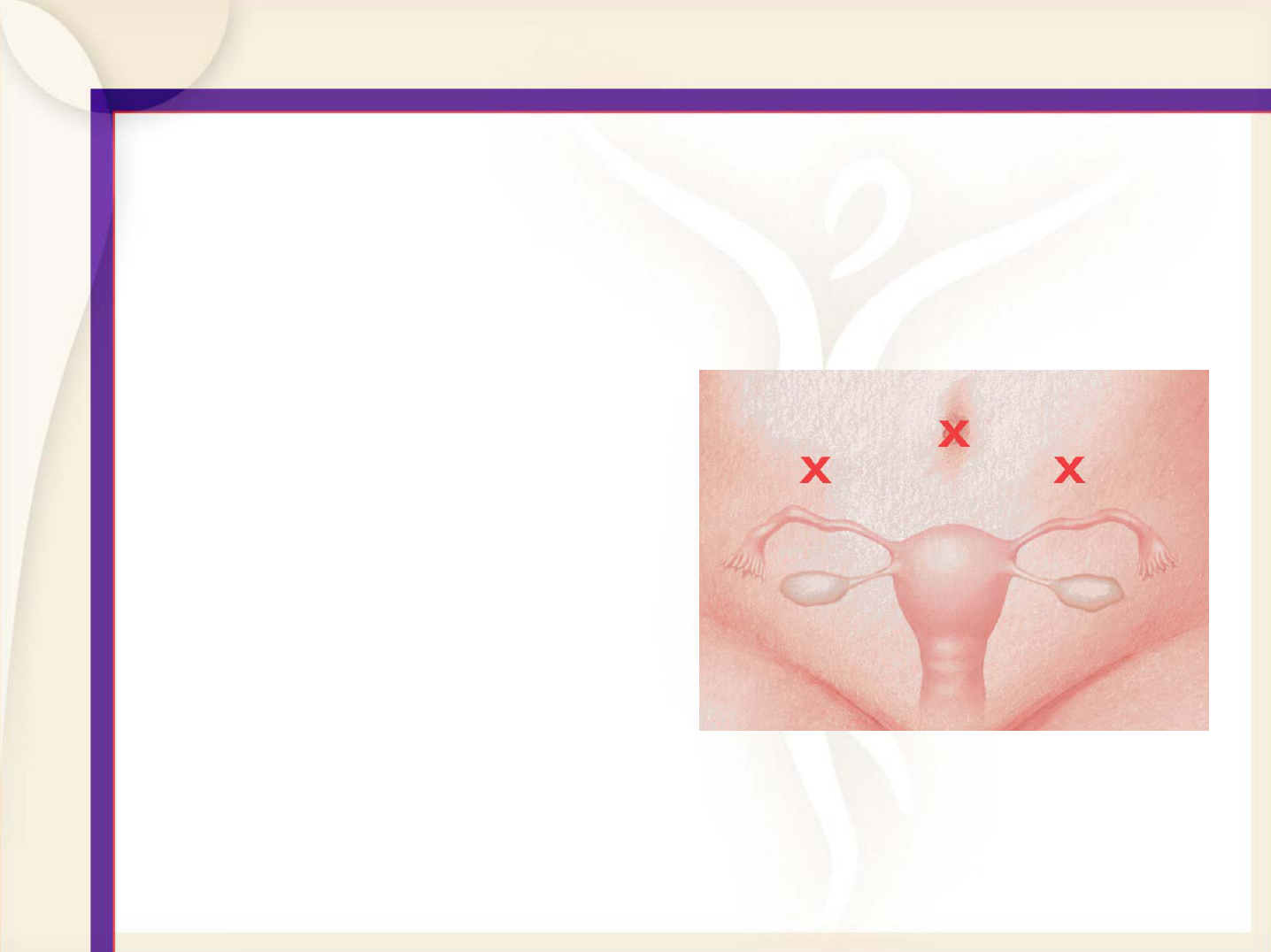
LSH Procedure
Hysterectomy Risks (for all types)
• All surgery involves risks
• Potential risks include blood loss, infection,
damage to internal organs
• Long-term complications may include
incontinence later in life
• Risks of general anesthesia
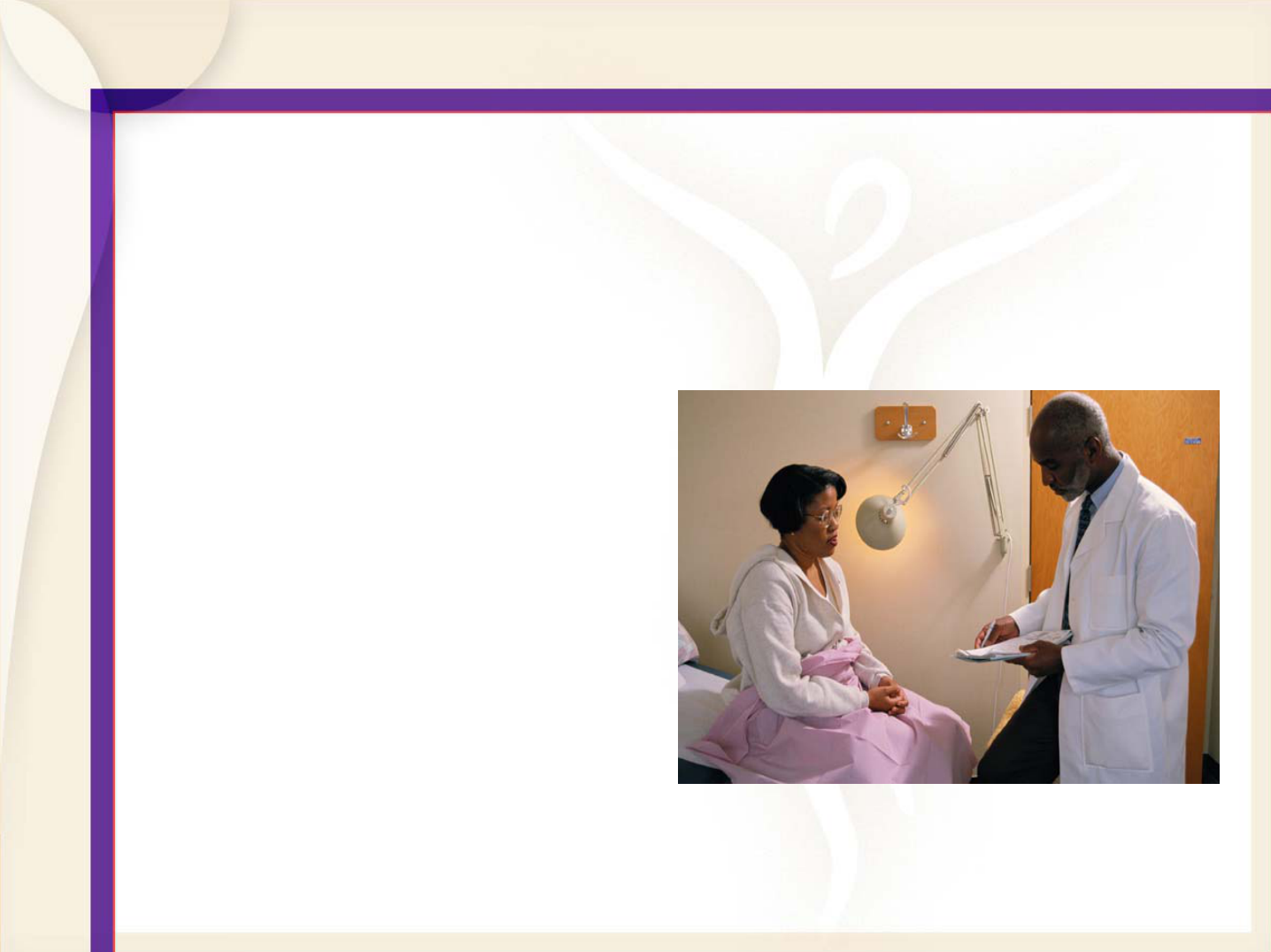
Know All of Your Options For Uterine Health
• There are many potential treatment options
• Get informed
• Talk with your doctor
Frequently Asked Questions
• How do I know what treatment option is best
for me?
• Can I get pregnant after any of these
treatments?
• Do any of these problems resolve
themselves?
• What are success rates of each medication
and surgical procedure available?
• What surgical alternatives do I have other than
hysterectomy?
Resources
Where you can find more information:
• www.healthywomen.org
(National Women’s
Health Resource Center -- NWHRC)
• www.acog.org
(The American College of
Obstetricians and Gynecologists)
• www.asrm.org
(American Society for
Reproductive Medicine)
• www.aagl.org
(The American Association of
Gynecologic Laparoscopists)
• www.apgo.org
(Association of Professors of
Gynecology and Obstetrics)